Overview
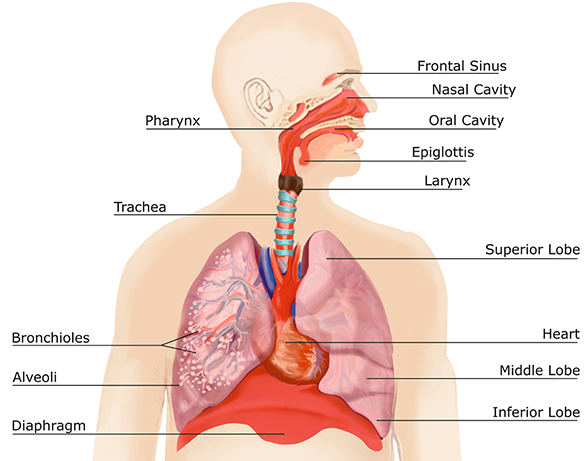
The human respiratory system is the network of organs and tissues that allow us to breathe by helping the body absorb oxygen from the air and clean waste gases like carbon dioxide from the blood. The airways, consisting of the mouth and nose, sinuses, throat, trachea, and bronchial tubes deliver air to the lungs, extract oxygen from the air and move it to the bloodstream. The bloodstream delivers oxygen to all the organs and tissues of the body.
The other parts of the respiratory system include:
- Alveoli: Tiny air sacs in the lungs where oxygen and carbon dioxide exchange occurs.
- Bronchioles: Small branches of the bronchial tubes that lead to the alveoli.
- Capillaries: Blood vessels in the alveolar walls through which the body exchanges carbon dioxide and oxygen.
- Lung lobes: Sections of the lungs — three lobes in the right lung and two in the left lung.
- Pleura: Thin sacs that surround each lung lobe and separate the lungs from the chest wall.
- Cilia: Tiny hairs that move in a wave-like motion to move mucus, with entrapped particulate matter and other irritants, up and out of the airways.
- Epiglottis: Tissue flap at the entrance to the trachea that closes when swallowing to keep food and liquids out of the airway.
- Larynx (voice box): Hollow organ that allows us to talk and make sounds when air moves in and out.
Measuring Changes in Airway Mucus
Normal airway mucus lines the epithelial surfaces (the cells that line the internal and external surfaces of the body) of the respiratory system. These surfaces are continuously exposed to the outside environment by breathing, eating, and speaking. Changes to airway mucus in reaction to external stimuli are a measurable biomarker during the physical activity of Forced Cough Vocalization (FCV) – that is, an intentional cough. This is the biomarker that RAIsonance technology captures, digitizes, and analyzes.
The primary defense used by airway epithelium is the secretion and clearance of mucus. Over time, humans evolved adaptations that created physiologic or biochemical methods to protect against airborne environmental hazards. Irritation of the respiratory tract causes changes in blood flow, mucus secretion, and the caliber – or diameter – of the airway. Toxins can interact with secretions directly and can lower viscosity, while sensory receptors in the body react to lung irritation or pulmonary inflammation. This inflammation changes both the quantitative and qualitative features of the sensory nerves.
Each of these responses to irritants changes the frequency and energy pattern of the FCV. Repeated or prolonged exposures to irritating gases, vapors, pathogens, and fumes can lead to the development of irritant-induced changes in the FCV. Laboratory studies confirm that airway inflammation creates cellular and tissue damage and can also lead to FCV changes.

Changes to airway mucus in reaction to external stimuli are a measurable biomarker during the physical activity of Forced Cough Vocalization (FCV) – that is, an intentional cough.
FCVs are a Critical Wellness Indicator.
Learn how our wellness products can improve your quality of life and safeguard your workforce.
Let’s discuss how we can help you >



